A major concern within the COVID-19 outbreak is hospitals’ supplies of personal protective equipment (PPE). To extend the use of current supplies, hospitals are considering sterilizing and reusing N95 respirators, as well as using respirators past their expiration date. That’s where Phillip Clapp, a research assistant professor at the University of North Carolina at Chapel Hill, and his colleagues come in.
The team at the Mucociliary Clearance and Aerosol Research Laboratory in the UNC Center for Environment, Asthma, and Lung Biology is measuring the effectiveness of different masks in filtering air particles. The have tested fitted filtration while a subject wears a mask and moves around — standing, bending, talking, or turning their head.
The team has discovered that reused, sterilized N95 respirators and expired N95 respirators retain their effectiveness at filtering particles like those that may contain the COVID-19 virus.
The researchers found that certain N95 respirators — as rated by the National Institute of Occupational Safety and Health (NIOSH) Administration — provide greater than 95 percent effectiveness at keeping the wearer from inhaling very small airborne particles that may carry SARS-CoV-2. Furthermore, these respirators retain effectiveness for years beyond their expiration dates and can be subjected to sterilization with hydrogen peroxide or ethylene oxide without compromising their efficiency.
Fitted filtration procedures showed that surgical masks with ties are approximately 70 percent effective at filtering inhaled particles, while surgical masks with ear loops are about 40 percent effective.
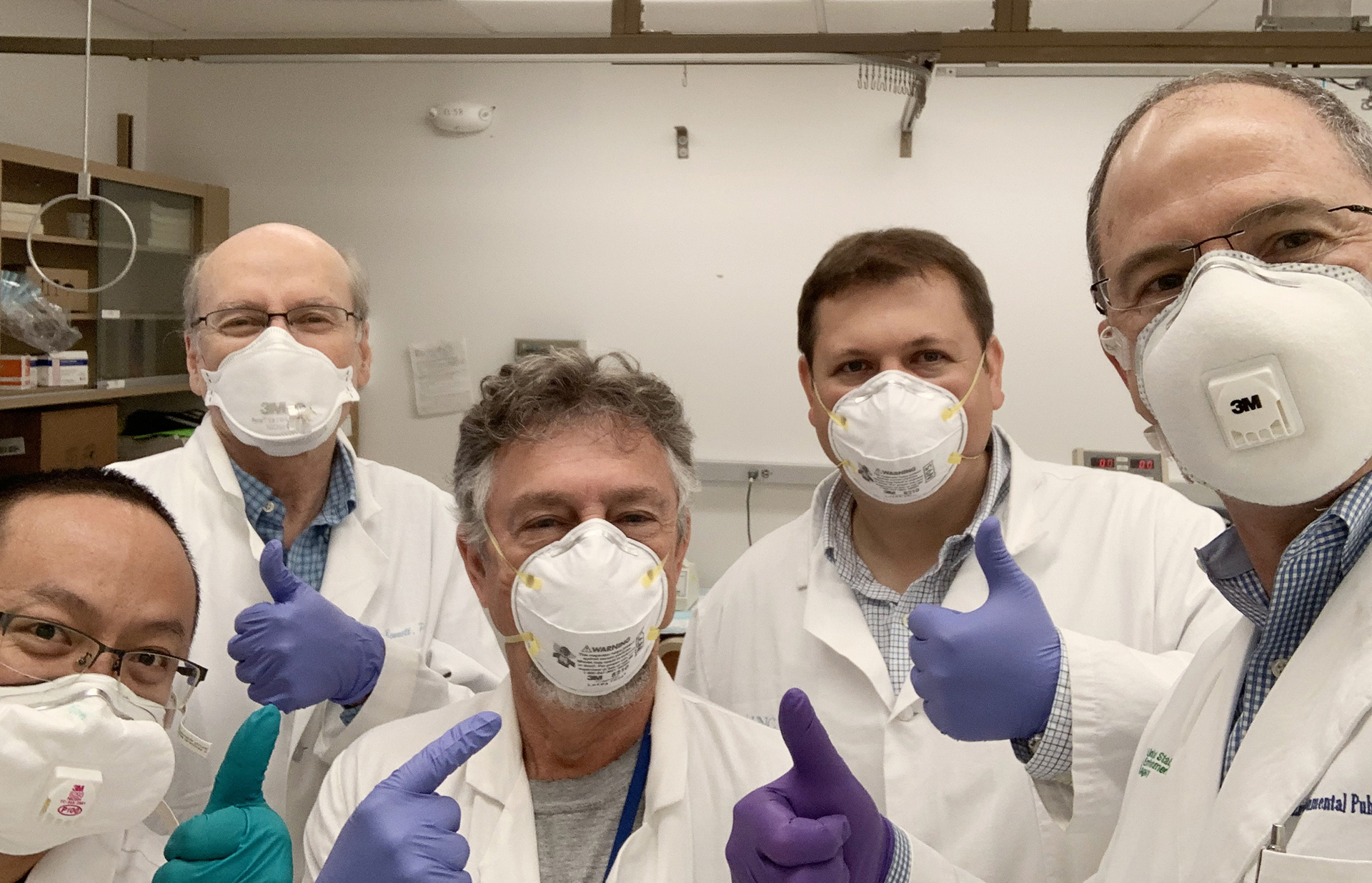 Hao Chen, William Bennett, Kirby Zeman, Phillip Clapp, and James Samet are part of the team testing the efficacy of a different face masks.
Hao Chen, William Bennett, Kirby Zeman, Phillip Clapp, and James Samet are part of the team testing the efficacy of a different face masks.
UNC Research: Why is it important to wear a mask, even if you don’t have COVID-19 symptoms?
Phillip Clapp: The idea behind this is that it protects others from you. This is important because, if you become infected, you may be able to spread the virus even before developing symptoms. Should you cough or sneeze, most of those droplets will be blocked by the mask, reducing the likelihood of transmission to others. It is most effective when everyone uses one because it reduces the spread of droplets from the wearer. You do not need a medical-grade respirator to protect those around you. Consumer-grade and homemade masks can be very effective at reducing transmission.
UNCR: What type of COVID-19 related research are you doing?
PC: In a true instance of serendipity, we discovered that a U.S. Environmental Protection Agency (EPA) research team working in the lab adjacent to ours was evaluating the effectiveness of various facemasks against environmental wood smoke. Using an exposure chamber filled with airborne particles, the investigators measured how many of those particles were able to penetrate each mask type to understand filtration efficiency. In a collaboration, we have tested the filtering efficiency of new, expired, and sterilized N95 respirators, non- certified but N95-labeled respirators, controlled air-purifying respirators, and surgical and procedural masks with ties and ear loops.
We have also been working with the UNC Department of Biomedical Engineering to develop ways to improve masks with poor filtering efficiencies like surgical or procedural masks. Additionally, after seeing all of the DIY masks being shared on the internet, I decided to include some of the most popular designs to see which were the most effective.
UNCR: What are some findings so far?
PC: Positive pressure-controlled, air-purifying respirators have more than 99 percent filtration efficiency. Unfortunately, these masks are also difficult to acquire under the current circumstances.
The expired N95s we tested, which were 11 years past their expiration date, filtered as well as the new respirators. But this may not be true for all expired respirators outside of UNC — the environment in which the masks are stored likely plays a large part in their efficacy.
We’ve investigated two forms of hospital sterilization: steam and ethylene oxide gas. Steam use may be questionable as one round of sterilization physically deformed one of the N95 respirator models, 3M 1860. But another model, 3M 1870+, was not altered and maintained its filtration efficiency after sterilization.
We also tested imported, non-NIOSH-approved KN-95 respirators. These products tested at approximately 80 percent effective, which does not meet the 95 percent filtration standard.
Perhaps most surprising was the low filtration efficiency of medical masks. Procedure masks with elastic loop ears functioned at about 40 percent filtering efficiency while surgical masks with tie strings had about 70 percent filtering efficiency. Unlike respirators, medical masks are not designed to fit tightly to the wearer’s face. Our data clearly show that the limited fit of medical masks impacts how well these products function as PPE.
A 12-year-old from British Columbia designed and 3D printed a device he called “ear guards” to make ear loop procedure masks more comfortable for hospital staff. I thought that an unintended result of using this device would be a tighter mask fit. Because this 3D-printer file was open-sourced, we were able to 3D print some for testing. Our first results showed that the surgical mask improved from 40 percent to 65 percent on a male and 27 percent to 88 percent on a female. This very promising, and we intend to do more testing.
UNCR: How did it come about to test DIY masks?
PC: As the severity of this pandemic in the U.S. increased, I started seeing DIY mask videos on social media and was curious as to how these homemade masks would compare to hospital-grade equipment.
Someone sent me a video on how to make a simple “no-sew” mask using blue shop towels — thick, durable paper towels found in auto supply stores. These masks were very simple to make and fit surprising well, so I decided to test them.
The shop towel masks were about 50 percent effective, but when we doubled the material to make a two-ply version of the mask, the filtering efficiency increased to about 75 percent. While neither the cotton or shop towel masks reached the effectiveness of N95 respirators, the data suggests they will provide some protection for the wearer and even more for those in the immediate vicinity of the wearer.
I should mention, though, that many of the materials people are using for DIY masks have not been evaluated for inhalation toxicity, and it is unclear whether some of these materials may cause harm. We are not suggesting or recommending that people use or not use any specific material for DIY mask making. Rather, we are only attempting to provide data for masks that are commonly used.
UNCR: What should people keep in mind when creating a mask?
PC: First, follow the CDC’s recommendation for face coverings and mask use. Second, most materials used for mask making have not been evaluated for inhalation toxicity. Third, with any mask, the key is to get a proper fit — even the best N95 respirator won’t protect you if it doesn’t fit appropriately.
On the other hand, don’t use masks that significantly restrict your breathing. I’ve been seeing online that people are making masks with multiple layers of material. Trying to breathe through a thick mask can be tough on your heart and lungs. This could put elderly people and those with preexisting cardiopulmonary conditions at risk. Don’t wear a mask that makes you feel like you’re suffocating and avoid wearing any mask for long periods of time.
Phillip Clapp is a research assistant professor in the Center for Environmental Medicine, Asthma and Lung Biology within the UNC School of Medicine.